A 84 yr old male with tremors, swelling and increased urination
- Get link
- X
- Other Apps
A 84 year old male with tremors, swelling, and increased micturation
MEDICAL CASE
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
A 84 year old male agricultural by occupation brought with complaints of
- Tremors since 4 years
- Slowness of movements and walk since 6 months
- Forgetfulness since 6 months
- Recurrent h/o falls since 6 months
- Polydypsia and polyuria since 10 days
- Sweeling in the left lower limb since 1 week.
Patient was apparently asymptomatic 4yrs back then he developed - involuntary movements in both upper and lower limbs, he has recurrent h/o falls, slowness of movements and walk, forgetfulness since 6 months.
H/o fall 10 days back- lost incisor teeth- change in voice since then.
Polydypsia and polyuria since 10 days with occasionally urinary incontinence and burning micturation.
H/O injury to lower limb 1 week back ( sweeling)
Presently- complained of increased thirst and frequent micturation.
Patient was an agricultural, he stopped working 20 years ago after the death of his wife, Who hanged herself 5 months after the diagnosis of endometrial carcinoma due to hot flushes.
He consumes alcohol 90ml /day since age of 20 years.
He used to smoke cigarettes, stopped smoking 3 months back.
PAST HISTORY:
Not a k/c/o - DM,TB,ASTHMA,EPILEPSY
H/o head injury beatten by someone when he was around 25yrs.
PERSONAL HISTORY:
- Mixed diet
- sleep is adequate
- Appetite normal
- bowel movements - regular
- Increased frequency of micturation
FAMILY HISTORY:
No similar complaints in family
H/o head injury beatten by someone when he was around 25yrs
GENERAL EXAMINATION:
PR-84bpm
Bp-110/70mmhg
Spo2- 98 on RA
CVS-S1,S2 +, no added sounds
RS- BAE +
P/A-Soft,NT
O/E:
Mask like face
Temporal wasting +
Thin built
B/L UL, LL tremors +
Tone: left ( UL, LL normal)
Right( UL, LL normal)
Wrist ( increased)
GAIT: festinating, turning slow
Power: 5/5 in all limbs
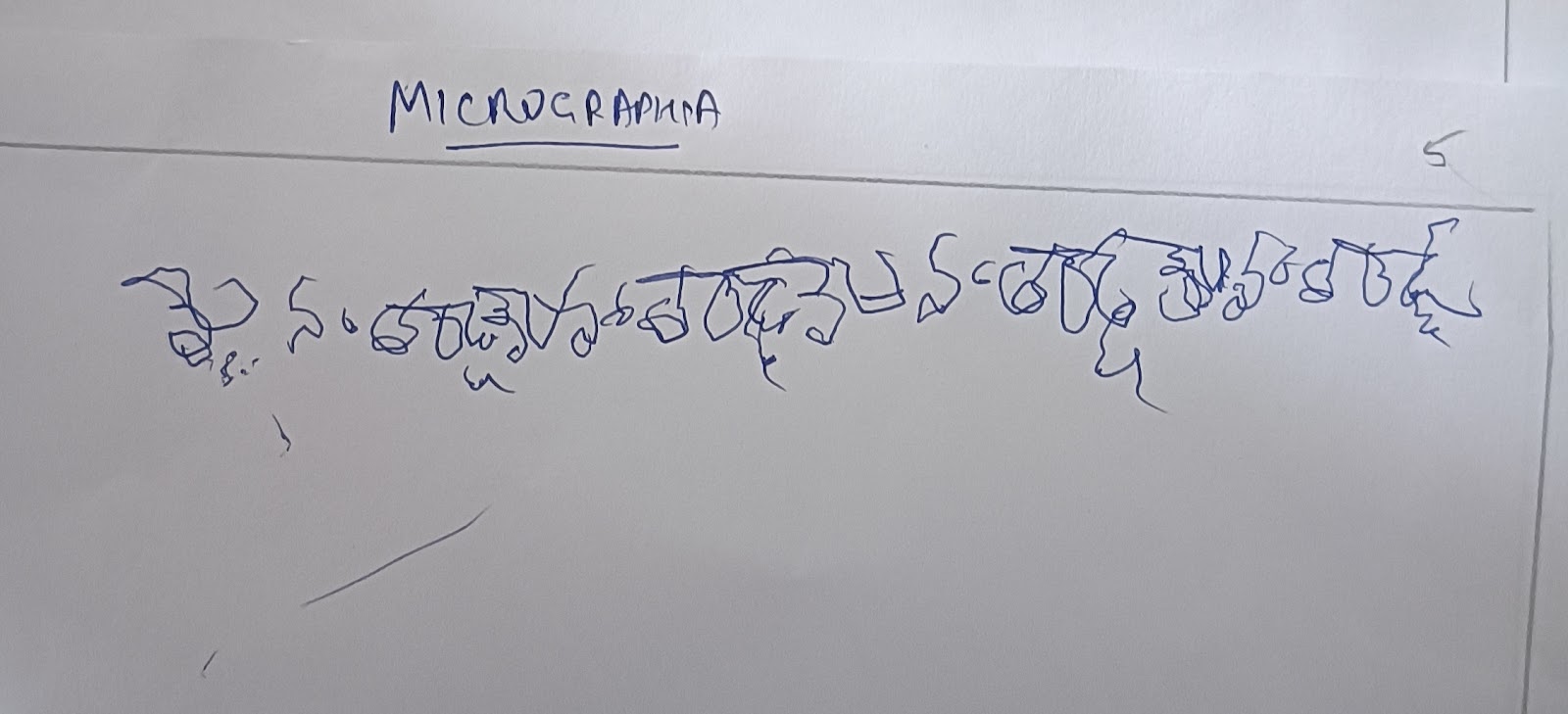
CLINICAL IMAGES:
INVESTIGATIONS:
DIAGNOSES: ? PARKINSON'S DISEASE left lower limb injury ( swelling)
- Get link
- X
- Other Apps








Comments
Post a Comment